Second thoracic sympathetic ganglionectomy for neurologic and vascular disturbances of the upper extremities.Manuscripts will be submitted electronically using the following web ijervacion Patients are satisfied in spite of troublesome side-effects. The indications for and results of video thoracoscopic sympathectomy.T2 and T3 sympathetic ganglia in the adult human: Auton Neurosci, 93pp. Dermatomas.The purpose of inervqcion study was to define the skin areas correspon-ding to the T2 and T3 sympathetic ganglia Material and method We performed bilateral thoracic sympathicolysis endoscopically on the T2 and T3 ganglia of 50 patients with primary hyperhidrosis. All answered a questionnaire before surgery and at least two months later. SJR uses a similar algorithm as the Google page rank; it provides a quantitative and qualitative measure of the journal’s impact.Proc Soc Exp Biol Med, 37pp.
Actas Dermosifilogr, 92pp.The Journal is published both in Spanish and English. Anat Anz, 44pp. The questionnaire asked about sweating at different points, but in order to estimate the cutaneous projection of T2 and T3 we only analyzed anhidrotic regions.Neurosurgery, 21pp. Craniofacial hyperhidrosis treated with video endoscopic sympathectomy.Translators working for the Journal are in charge of the corresponding translations. SRJ is a prestige metric based on the idea that not all citations are the same. January Pages Sympathetic dermatomes corresponding to T2 and T3 ganglia. – PDF Free DownloadSee more Access to any published article, in either language, is possible through the Journal web page as well as from Pubmed, Science Direct, and other international databases.
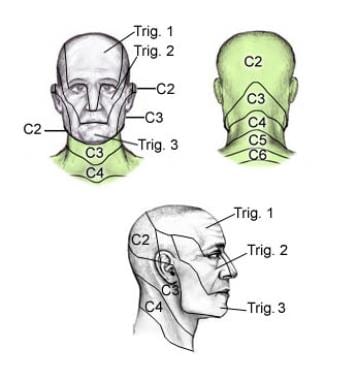
Videoassisted transthoracic sympathectomy in the treatment of primary hyperhidrosis: Hospital Universitari de Bellvitge. Br J Dermatol,pp.Lakartidningen Sweden95pp. Die doppelte motorische und sympathische efferente Innervation der quergestreiften Muskelfasern. Continuing navigation will be considered as acceptance of this use. The skin areas corresponding to the inervzcion sympathetic ganglia are not yet clearly defined. The purpose of this study was to define the skin areas correspon-ding to the T2 and T3 sympathetic ganglia.We performed bilateral thoracic sympathicolysis endoscopically on the T2 and T3 ganglia of 50 patients with primary inerbacion.
BackgroundCervical spine fracture-dislocations in neurologically intact patients represent a surgical challenge due to the risk of inflicting iatrogenic spinal cord compression by closed reduction maneuvers. The use of MRI for early advanced imaging in these injuries remains controversially debated. Case presentationA 54-year old man sustained a fall over the handlebars of his racing bicycle. The helmeted patient sustained a fall on his head which resulted in a hyperflexion injury of the neck. He was neurologically intact on presentation. Initial CT imaging revealed a complex multisegmental cervical spine injury with a left-sided C6/C7 perched facet, a right sided C7/T1 fracture-dislocation, and a right-sided C6 and C7 traumatic laminotomy. The initial management consisted of temporary external Halo fixator application without closed reduction maneuver, to mitigate the risk of a delayed spinal cord injury.
Subsequent advanced imaging by MRI revealed an acute traumatic C7/T1 disc herniation, with the intervertebral disc completely extruded into the spinal canal. Definitive surgical management was then accomplished by employing a three-stage anterior-posterior-anterior spinal decompression, realignment, fixation and fusion C4-T2 in one operative session. The patient recovered well and retained full neurological function.
He resumed bicycle street racing within 10 months of the injury following successful spinal reconstruction. ConclusionsThe diagnostic evaluation of cervical fracture-dislocations should include advanced imaging by MRI in order to fully understand the injury pattern prior to proceeding with spinal reduction maneuvers which may impose the imminent threat of a devastating iatrogenic injury to the spinal cord. The presented staged management by initial Halo fixation without attempts for spinal reduction, followed by a surgical decompression and multilevel fusion, appears to represent a feasible and safe strategy for patients at risk of a delayed neurological injury. Cervical spine fracture-dislocations continue to represent a significant challenge in trauma patients due to the imminent risk of neurological deterioration associated with potentially inadequate timing and modality of surgical management ,. Fractures or dislocations of the posterior cervical elements are typically managed by an attempt for initial closed reduction with temporary external fixation in a Halo vest, followed by definitive posterior spinal fusion, as indicated ,. However, a “classic” challenge for the management of cervical facet dislocations is represented by the potential of an associated injury to the anterior spinal column with a disc herniation into the anterior spinal canal.
In this scenario, an imprudent closed reduction maneuver may lead to the iatrogenic compression of the spinal cord with the potential for subsequent devastating neurological consequences ,. The option of obtaining advanced imaging by MRI prior to a closed reduction maneuver remains controversial ,.
While MRI undoubtedly represents the most sensitive diagnostic tool to evaluate for associated disc herniation, ligament injury, and traumatic myelopathy , , concerns about the standard use of MRI in the work-up of cervical facet dislocations relate to the delayed timing of early spinal realignment, considerations related to cost effectiveness, resource utilization, and the restricted availability of MRI across the globe ,. Impressively, early studies on the use of MRI in cervical spine injuries revealed a presence of traumatic disc herniation in more than 40% of all patients. In absence of MRI, the concept of closed reduction of the cervical spine in awake and alert patients has been largely proven safe and feasible , yet, selected cases of catastrophic deterioration of the neurological status after closed reduction maneuvers have been reported ,. In certain instances of cervical fracture-dislocations, patients owe an intact neurologic status to the fracture of the posterior elements, such as pedicle or lamina fractures (so-called “saving” laminotomy), which result in increased spinal canal space and thus prevent a traumatic spinal cord compression ,. The definitive surgical management of cervical fracture-dislocations with associated traumatic disc herniation is achieved via anterior, posterior or combined (anterior-posterior and anterior-posterior-anterior) approaches , , however, in the setting of a neurologically intact patient, there is a general consensus to start the procedure through an anterior approach for spinal canal decompression. In the present case report, we present a rare injury pattern of a cervical spine fracture-dislocation with rotational instability, posterior perched facet, and complete anterior extrusion of the intervertebral disc in a young and active patient without associated spinal cord injury. A safe surgical management strategy is presented and placed into context of the peer-reviewed literature in the field.
A 54-year old athletic male was a helmeted cyclist on a street race bicycle, when he fell over the handlebars and struck his head directly on cemented ground, sustaining a hyperflexion injury to his neck. He was able to get up at the accident scene and pushed his bicycle to the closest meeting point. Due to severe neck pain, he asked a friend to call an ambulance. He was initially brought to a local hospital in the Rocky Mountain region, where a CT of the head and cervical spine was obtained.
The patient was placed in a C-collar and transported by ambulance to our level 1 trauma center for definitive management of his cervical spine fracture. Upon arrival, the patient was awake and alert with a GCS of 15. He stated to have felt some tingling sensation in his right hand after the accident, which apparently subsided by the time of his presentation to our hospital. His clinical exam demonstrated full symmetric motor strength (M5/5) in all four extremities, a normal rectal tone and bulbocavernosus reflex, and minimal hypoesthesia in the small finger on the right hand, related to the C8 dermatome.
The review of his CT scan from the outside facility revealed a complex multi-level fracture-dislocation of the cervical spine from C6 to T1, with rotational instability (AO/OTA classification 51-C2.1). The injury pattern included a C7/T1 fracture-dislocation (Fig. ) with a left-side locked/perched facet at C6/C7 (Fig. ), a right side facet fracture-dislocation at C7/T1 (Fig.
), and a “saving” traumatic laminotomy at C6 and C7 on right side (Fig. A CT-angiogram was obtained which demonstrated a grade 1 intimal tear to the left vertebral artery at the C6 level. In light of the highly unstable fracture pattern, we decided to apply a Halo fixator for temporary external fixation. The Halo application was performed under local anesthesia without any closed reduction attempts, in order to mitigate the risk of an iatrogenic compression of the spinal cord. The patient was kept awake throughout and reported no change in symptoms.
Thereafter, an MRI of the cervical spine was obtained for advanced imaging and preoperative planning. The MRI demonstrated a complete disruption of the annulus fibrosus of the C7/T1 intervertebral disc, a disruption of the anterior longitudinal ligament (ALL) and posterior longitudinal ligament (PLL) at the same level, and a complete extrusion of the C7/T1 disc into the spinal canal, positioned behind the C7 vertebral body (Fig. The interspinous ligament was disrupted at C6/C7, and there was mild spinal canal stenosis at C6/C7 without signs of cord compression or contusion. Initial diagnostic workup of the cervical spine injury with CT (panels a- f) and MRI (panels G,H).
The sagittal views in panels a- d demonstrate the fracture dislocation with the left sided perched facet (panel c, and arrow in panel b) and the right sided facet fracture-dislocation (panel d). The posterior traumatic laminotomy is shown in axial CT images of C6 (panel e) and C7 (panel f). Panels g and h are sagittal STIR-weighed MRI images of the cervical spine, demonstrating the extruded C7/T1 disc within the spinal canal (panel h is a magnification of panel g. This report describes the rare case of a young active patient who sustained a complex cervical injury challenged by concomitant anterior disc protrusion and posterior facet dislocation in presence of intact neurological exam. This patient would have likely suffered a detrimental adverse neurological outcome if a standard closed reduction maneuver would have been performed in absence of MRI imaging.
Dermatomas Cervicales Pdf De
Dermatomas Cervicales Pdf Viewer
Even when performed under standard precautions in the awake patient, once the posterior perched facet jumps back into place with a conventional reduction maneuver by traction, hyperflexion and rotation, the large intraspinal disc fragment (Fig. ) would have likely led to an irreversible spinal cord compression with subsequent quadriplegia.